Cirrhosis and ACLF
Up to 30 liver centres across Europe will participate in the clinical study of A-TANGO. Soon, we will add a page where you can view all study sites and search for the closest participating liver centre.
Cirrhosis & Decompensation
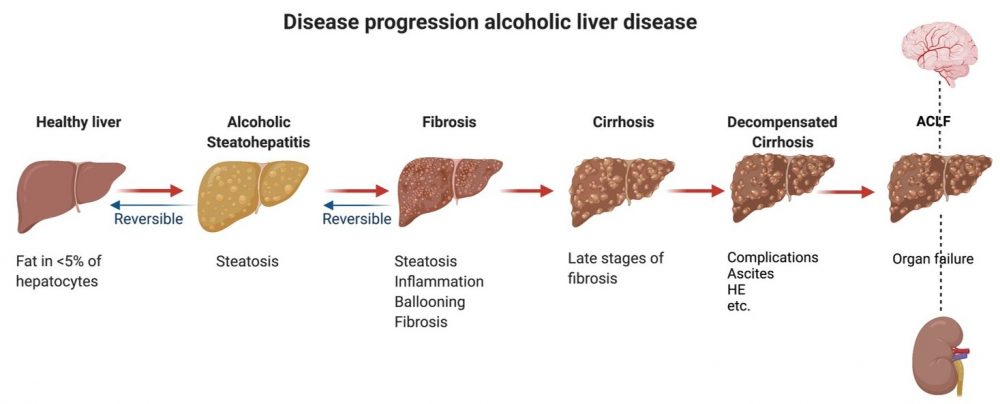
Liver diseases that lead to cirrhosis, in other words scarring of the liver, include autoimmune disorders, fatty liver, as well as bacterial or viral infections. Alcohol abuse, however, accounts for the majority (30-40%) of all liver-related deaths in Europe. A severe form of alcoholic liver disease is called alcoholic hepatitis (sAH), which carries high mortality rates. Regardless of the cause, when cirrhosis progresses too far, the body can no longer compensate for the dysfunctional liver. This results in fluid accumulation in the abdomen (ascites), impaired brain function (hepatic encephalopathy), and bleeding (gastro-intestinal hemorrhage).
Acute-on-Chronic Liver Failure (ACLF)
Untreated, decompensated cirrhosis eventually leads to acute-on-chronic liver failure (ACLF) and death. Aside from enormous individual suffering, ACLF has a major socio-economic impact because of high health care costs and the patients’ inability to work or seek employment. Currently, an alarming 30-40% of the patients that suffer from ACLF die within three months. Treatment options are still limited, leaving liver transplantation as the last resort. Thus, effective treatment approaches are an urgent need in order to decrease the mortality rate of patients with ACLF. Research has demonstrated that ACLF is caused by inflammation and the inability of the liver to regenerate. The high mortality rate of ACLF is related to the dysfunction and failure of multiple organs. Accordingly, ACLF has been defined as “a condition characterized by acute deterioration of a cirrhotic patient with or without a recognized precipitating event, associated with organ failures and high mortality rates distinguishing this condition clinically and pathophysiologically from decompensated cirrhosis” (Jalan et al. 2014). Furthermore, ACLF occurs in middle-aged patients (average age 52 years) and about 50% have no knowledge of their underlying cirrhosis. Alcoholic cirrhosis and associated alcoholic hepatitis accounts for more than 50% of the cases of ACLF. ATANGO focuses on the group of patients with srAH associated with ACLF.
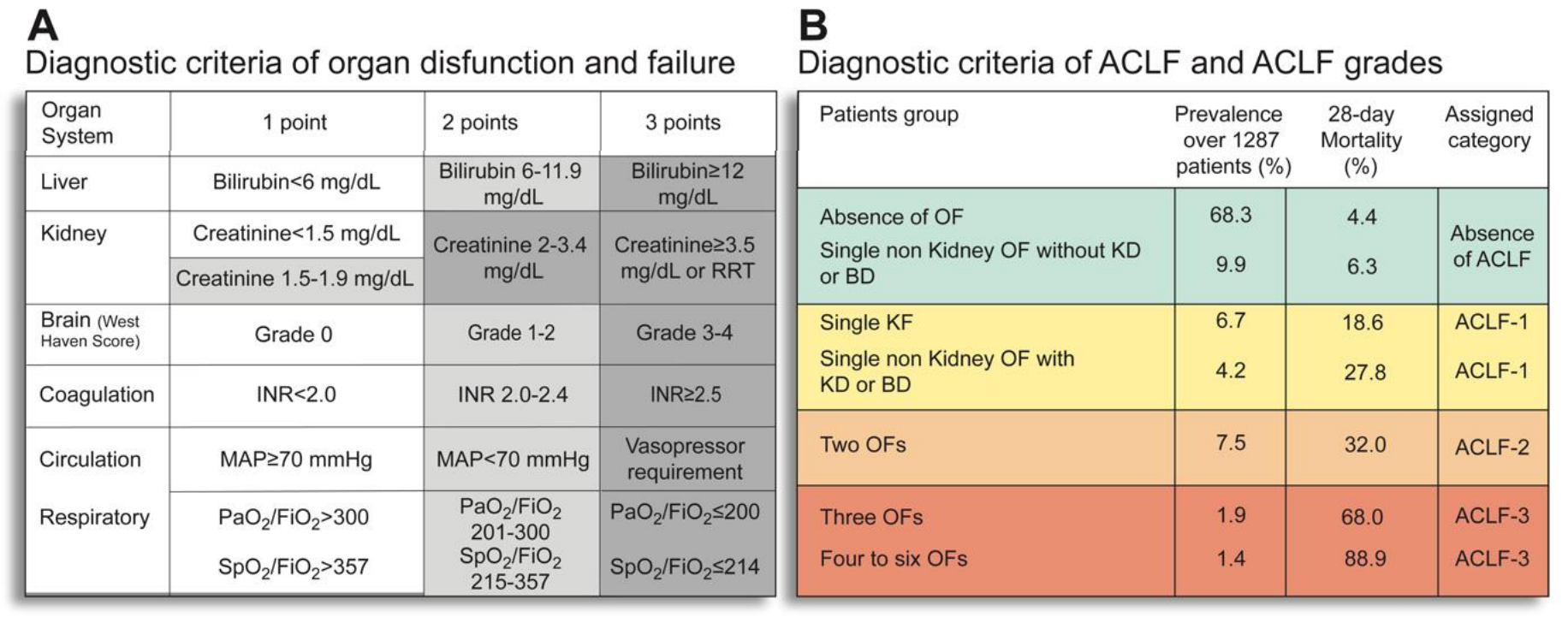
ACLF Symptoms & Diagnostic Criteria
The members of the A-TANGO consortium have developed new and validated criteria for defining the diagnosis and prognosis of these patients allowing performance of clinical studies of novel interventions to reduce mortality. The diagnosis of ACLF is made using the CLIF consortium organ failure score (CLIF-C OFs) and the prognosis of these patients is assessed using the CLIF consortium ACLF score (CLIF-C ACLFs). For details see Moreau et al. 2013 and Jalan et al. 2014. A-TANGO consortium members have shown that ACLF outcomes are highly variable: about half patients with early grades of ACLF improve while about 30% progress to the more severe grades (Gustot et al. 2015).